School’s out for summer and if you have any concerns about your child’s health or wellbeing, you might be wondering where you can get support. Dr Ashutosh Joshi, a Consultant Paediatrician in London, shares his advice to help.
1. Be alert for measles

Measles is currently circulating in the UK and across Europe. It’s highly contagious and 9 out of 10 unvaccinated children will catch it if they come into close contact with someone who has it. It could make them seriously ill and weaken their immune system for a few years after infection.
Measles usually starts with cold-like symptoms (such as a high temperature, runny or blocked nose, sneezing and cough) followed by a rash a few days later.

“1 in 5 children will need a hospital visit as it can also lead to serious complications including pneumonia (severe chest infection), meningitis (brain infection), sepsis and in rare cases death,” warns Dr Joshi.
If a family member has measles, call NHS 111 if they are getting more ill rather than better. And take steps to avoid passing it on to anyone at higher-risk from measles, such as unborn and young babies, older people and people prone to infections. Children should stay away from school for at least 4 days from when the rash first appears.
2. Protect your family against serious diseases

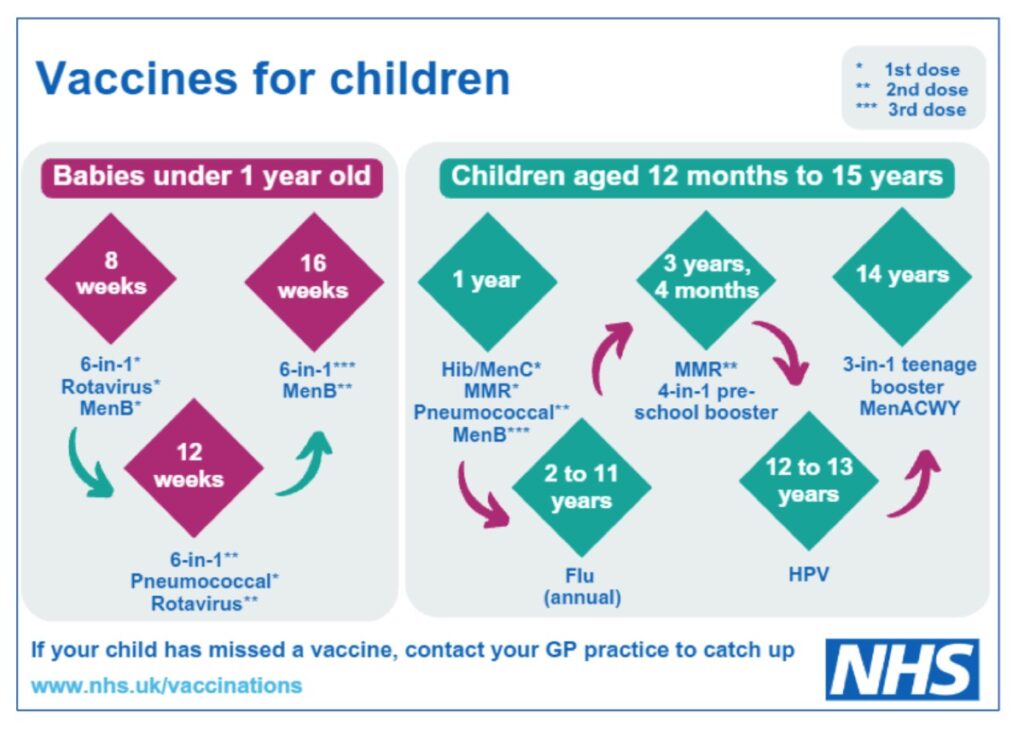
Two doses of the MMR vaccine will provide lifelong protection from measles, as well as mumps and rubella. Dr Joshi explains vaccination is the best protection against becoming seriously ill from measles, which also has no medical treatment.
“Since the measles vaccine was introduced in the UK in 1968, 20 million infections have been avoided and 4,500 lives have been saved. And the more people that have the MMR vaccine, the more protected our whole community becomes.
“Vaccines protect us from life-changing diseases, at stages of our lives when we most need them. This includes in pregnancy, childhood, and in our later years,” explains Dr Joshi.
You can check which vaccines your child has had in their child personal health record (also known as the red book) and contact your GP practice to book any they may have missed.
Read more about vaccinations at nhs.uk/vaccinations
‘Print out and keep’ pod
3. Watch out for changes in their mood and behaviour

Encouraging our children to share how they are feeling is important, explains Dr Joshi. “Gadget-free evening meals, provide a great time to chat and have wellbeing conversations. If something doesn’t seem right, try and find out what’s troubling them – without judging them or their actions.
“Let them know you’re there to listen and support them, or they can talk to a teacher, trusted adult, friend or get advice online at youngminds.org.uk.
- Depression
Children can get depressed too and symptoms include low moods, tearfulness, irritability, not enjoying the things they used to and disturbed sleep.
- Anxiety
While anyone can feel worried or anxious at times, notice if it affects your child’s wellbeing or ability to do everyday things. Symptoms include being irritable, tearful or clingy, wetting the bed or sleep problems, in some children, it might also show as stomach problems. Older children may find it hard to concentrate, have angry outbursts or negative thoughts and avoid their normal everyday activities.
- Eating disorders
An eating disorder is a mental health condition where controlling food intake is used as a way to cope with feelings. Warning signs include significant weight loss, lying about how much they have eaten, going to the bathroom a lot after eating and spending time worrying about weight and body shape.
4. Seek early help for learning or development disabilities

Learning and development disabilities can affect how someone learns new things and understands information.
There are many possible causes, including autism and if you’re worried about your child’s development or feel they aren’t reaching milestones from their red book, you can ask for help. Dr Joshi says, “If you think your child may be autistic, ask your GP practice or school nurse for an autism assessment. This is the first step towards a diagnosis.
“The support your child needs will be very individual. For example, one autistic child may need help with communication, whilst another might need other types of support.”
Anyone with a learning disability should be included on the GP learning disability register, and this should mean they’re offered an Annual Health Check (AHC) from the age of 14 years. You can ask your GP practice to arrange an AHC, and to make sure your child is on the register.
5. Supporting your child with a long term condition
When she was just 4-months-old, Roanna Maharaj’s parents got the news she had thalassaemia. She tells us about living with a long term condition and the importance of her parent’s support: “Whilst we were living in Trinidad and Tobago, my mother said I had gone from a being a feisty new-born; full of life and smiles to a lethargic baby, who was no longer feeding well.
“She instinctively knew something was wrong and pleaded with paediatricians to find out why.” It took doctors five-weeks to diagnosis a severe form of beta thalassaemia major that needed an emergency blood transfusion.
Although many people haven’t heard of the condition, there are 1,700 people in England living with this rare blood disorder and approximately 300,000 silent carriers. Thalassaemia affects how much haemoglobin our bodies produce, which is used by red blood cells to carry oxygen around the body.
“To control my severe symptoms, I require life-long blood transfusions every 2 weeks, and copious amounts of medications to treat iron overload and secondary conditions acquired. In 2011, I began reacting to my life saving blood transfusions and during one of my most severe spells in 2016-2018, I was virtually housebound. I needed a Zimmer frame to walk, a break during showers and needed help to feed myself.
“To help me get better during those 2 years, I received 248 units of blood. This was difficult, as I needed ‘matched blood’, and there weren’t enough black and Asian donors in England to accommodate this. Did you know it’s so simple and easy to donate blood and save lives, so I’d encourage those that can, to register at www.blood.co.uk.“
Thalassaemia mainly affects people from South Asian, Mediterranean and Middle Eastern origins. If both parents carry the gene, it can be passed to the baby, so is often detected through screening during pregnancy or soon after birth with a heel prick test. If you’re trying for a baby or expecting soon, it’s important to find out your carrier status by speaking with your GP practice or midwife. Early diagnosis means earlier treatment, to improve the quality of life for both parents and children.
“I’m determined to live my life to the fullest and I’m blessed to have my family’s support. Despite the challenges, I have completed my undergraduate and graduate professional training in clinical health psychology and continue to advocate and support others living with thalassaemia and other genetic blood conditions.”
Find out more from the UK Thalassaemia Society (UKTS)

Roanna is a psychologist practitioner and public speaker, with a special interest in genetic conditions and rare diseases.
To get help so you can support your children’s feelings, behaviours, development or long term conditions, talk to your GP practice, your child’s school, another healthcare professional or call NHS 111. For more information, search nhs.uk.