
“If your parent, grandparent or sibling has type 2 diabetes, you can reduce your own risk by taking extra care of your weight, diet and lifestyle.”
Produced in Partnership with the NHS

Our heart health
Research shows first-generation South Asians living in the UK have twice as much risk of getting coronary heart disease. And although a third of adults in the UK have high blood pressure, it disproportionately affects people from ethnic minority backgrounds.
Many of us have a friend, colleague or family member who has diabetes, heart disease or high blood pressure.
“A healthier lifestyle could reduce our risk of type 2 diabetes, while being alert for symptoms, could help you get advice, treatment and support much sooner,” says Professor Partha Kar, a consultant in Diabetes and Endocrinology in Portsmouth and the NHS’s National Diabetes Advisor.
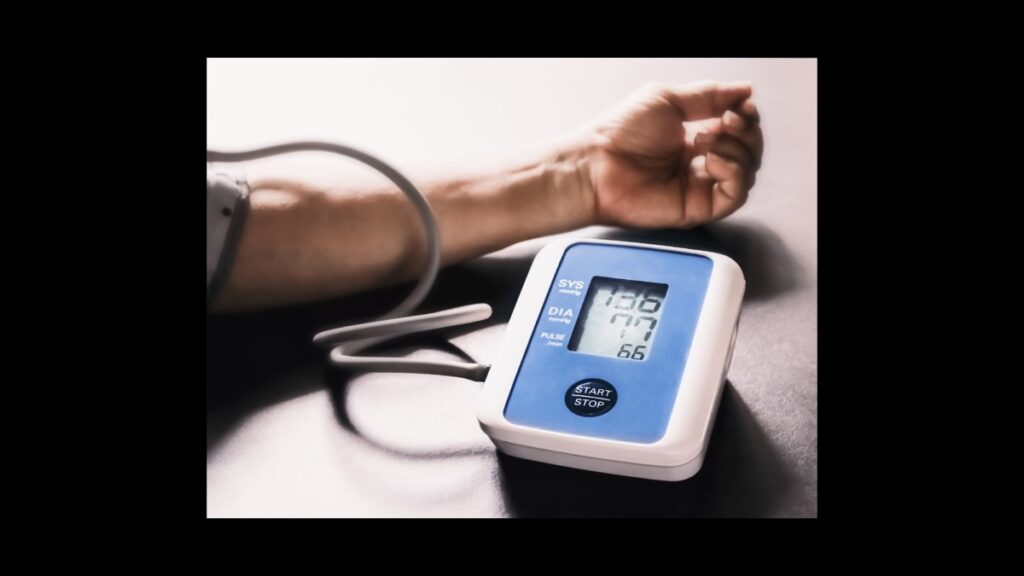
High blood pressure doesn’t have obvious symptoms, but it significantly increases the risk of heart attack or stroke.
Added to this, people from South Asian backgrounds up to 6 times more likely to develop type 2 diabetes and we’re more at risk after the age of 25. The risk for white Europeans is much lower and increases after the age of 45 years.
Why is our risk of type two diabetes higher?
It’s not clear why some people are more likely to be affected than others. Our age can play a part. As we get older, the pancreas can become less effective at doing its job. Professor Kar explains our risk may be linked to lifestyle and where fat is stored in our body.
“People from a South Asian background, tend to store fat in the middle or tummy area of our body. This fat is known as visceral fat and it’s close to major organs like the pancreas and liver. The amount of visceral fat we have has been linked to increased risk of conditions like type 2 diabetes or heart disease.”
Being less active and regularly eating foods that are high in sugar, fat and salt increases visceral fat. While the salt can also cause high blood pressure and heart related problems. A particular worry for those with a busy life and an over-reliance on the convenience of processed and fast food.
“We need to be mindful about the types of food we eat, the impact it may have and how often we eat them, to avoid known risks to our health. If your parent, grandparent or sibling has type 2 diabetes, I’d advise you to pay particular attention to your weight, diet and lifestyle”.
Professor Kar adds: “Weddings and parties come with generous helpings of fried snacks. Although we all love a samosa or two, eating fried food on a regular basis can contribute to weight gain and other problems.”
Research shows British South Asians, particularly women, tend to be less physically active than the white British population. People who aren’t active, and those who are overweight or obese, are more likely to develop type 2 diabetes. The COVID-19 pandemic meant many of us became more inactive, with less exercise and more time at home.
Symptoms of type 2 diabetes

Symptoms can vary and some people have mild or no symptoms at all, making it harder to spot. Common symptoms include:
- feeling more hungry or thirsty
- urinating more than usual, especially at night
- feeling very tired
- losing weight without trying
- blurred vision
- numbness or tingling in hands or feet
- sores that don’t heal
Type 2 diabetes can take years to develop. Some people only find out they have it when they develop related health problems, like heart disease or concerns with their sight. If you’re worried about risks or symptoms, your GP practice can arrange tests to check your blood sugar levels and give you help and advice.
Living with diabetes
If you have, or are at risk of type 2 diabetes, you can reduce chances of other complications by leading a healthy lifestyle. A free online NHS service called Healthy Living is proven to help participants with information and advice.

Kirit Mistry, a health equalities and diabetes community champion from Leicester raises awareness about health topics affecting South Asian communities. He has type 2 diabetes and advises: “The most important way to control my diabetes is with better self-care and management. I follow medical advice, try to eat a healthy diet and make sure I stay active. And taking medication at set times of the day helps to manage my blood glucose levels.”
If type 2 diabetes is left untreated, it can lead to other health complications, including kidney failure, loss of vision or a limb and can increase the risk of a heart attack or stroke.
Kirit adds: “As diabetics, we are vulnerable to infections which can make us seriously ill and take us longer to recover. When I was invited for my flu and COVID-19 vaccines this winter, I booked them both to stay protected.”
Everyone aged 12 years and over who have either type 1 or type 2 diabetes is also offered diabetic eye screening. It’s important, as it checks for eye problems which can lead to sight loss if not found early. For more information about these and other NHS screening programmes, visit www.nhs.uk
What are type 1 and type 2 diabetes?
Our blood sugar levels are regulated by a hormone called insulin which is made in our pancreas. If it isn’t doing its job correctly, our bodies may not produce any or enough insulin, causing our blood sugar levels to go too high. There are two types of diabetes:
Type 1 diabetes is a genetic, lifelong auto-immune disorder, usually diagnosed in childhood and unrelated to lifestyle. The immune system attacks and destroys the insulin-making cells in the pancreas, so it doesn’t produce the insulin needed to control blood sugar levels.
Type 2 diabetes is more common, particularly with South Asian communities. Here, insulin in our bodies doesn’t do its job properly or the pancreas doesn’t make enough of the hormone. Unlike type 1, it is often related to lifestyle and usually detected later in life. It can sometimes be prevented or reversed if caught early.
Reduce your risk of type 2 diabetes

- Stay active: At least 150 minutes of physical activity a week will help to lower your risk of long-term conditions and support mental health.
Eat healthy: A well-balanced diet with smaller portions helps to reduce our risk of health problems. It’s sensible to include plenty of fruit and vegetables and avoid foods with high levels of sugar, fat and salt.
Lose weight: You may be able to prevent or delay diabetes by losing weight and reducing your waist measurement.
Blood pressure checks: Everyone over the age of 40 should have their blood pressure checked regularly by your GP practice or one of many local pharmacies.
Check your risk online: If you have a family history of type 2 diabetes or have some of the common symptoms, you can check your risk by using Diabetes UK’s online ‘Know Your Risk’ tool. - Ask about the Healthier You NHS Diabetes Prevention Programme: Your GP practice might refer you to this programme if you are at moderate or high risk of developing type 2 diabetes. Over one million people in England have been referred and supported with simple, sustainable lifestyle changes to significantly reduce the risk of developing diabetes and even, in some cases, reverse type 2 diabetes
You can find out more about COVID-19 vaccinations and book what you are eligible for at nhs.uk/COVIDvaccine, by calling 119 (translators are available) or by scanning the QR code below, or find out more about the NHS services at www.nhs.uk/nhs-services.
















